A better way toprior-authorize.
Itiliti Health’s best-in-class technology revolutionizes the prior authorization process. By clearly communicating payer rules to providers and by leveraging interoperability and automation, Itiliti Health delivers a touchless prior authorization process that is fast and efficient.
A new era of Medical Policy Optimization
Our solutions address the need to modernize the processes and management of prior authorizations for payers. The result is a CMS #0057-F compliant solution that delivers an improvement in patient care and significant reduction in administrative cost.
Our Products
Constructed with a flexible, open-API framework, our suite of products is designed to offer a comprehensive solution for automating prior authorizations, or it can be tailored to meet specific needs through its individual components.
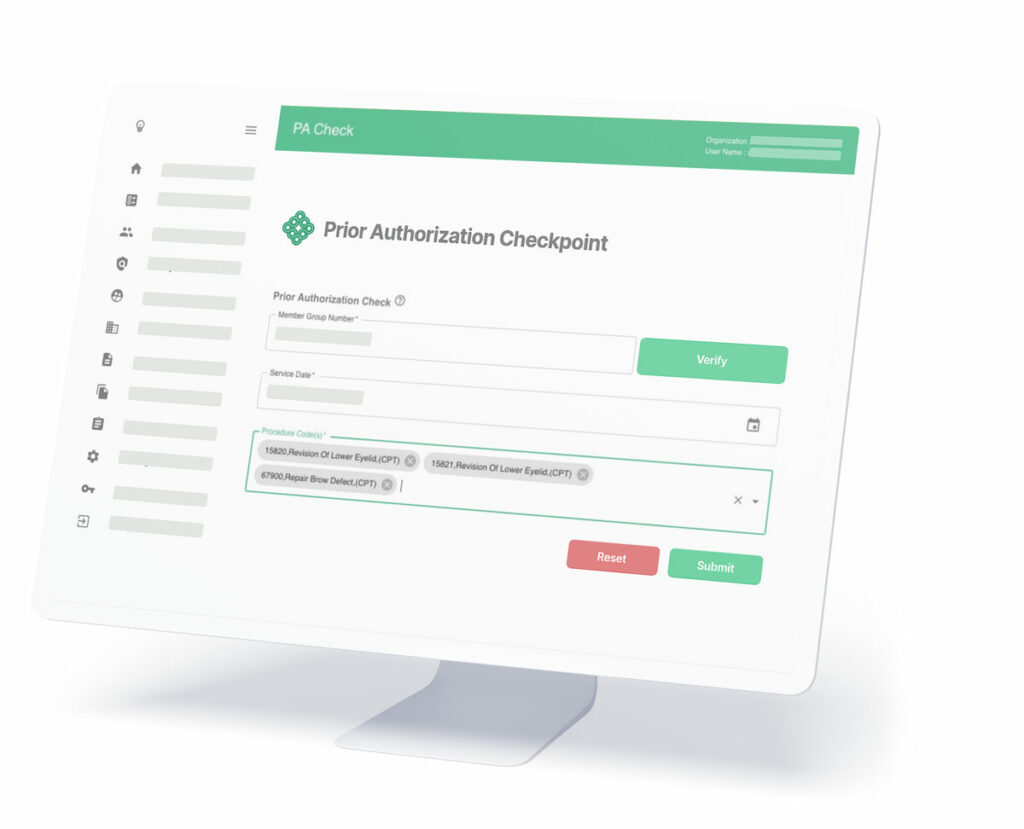
- PA Checkpoint™: Is Auth Required? and Policy Transparency
- Policy Management
- Prior Authorization Routing
- Automatic Authorization Rules
- Clinical Decision Assistant
ROI Seen By Our Customers
$5 million per year in administrative cost savings
30% reduced prior auth submissions
20% reduced call volume + 15% reduced call times
Near elimination of prior auth disputes
Over 6,000% reduction in misquote costs
And more!
Ready to create similar ROI for your organization?
Request a demo with our team:
Payers
Providers
The right answer,right away
At Itiliti Health, we apply cutting edge technology and interoperability standards with our deep understanding of user experience to offer a platform that eases administrative friction and workflow for plan administrators and physicians.
Streamline Prior Authorizations
Itiliti Health’s suite of transparency and automation products will reduce your costs while increasing the satisfaction of both providers and your staff.
Our solutions are:
- HIPAA certified
- Utilize modern APIs and standard data structures
- Can be implemented in under 60 days
About Itiliti Health
Our team is relentless in their pursuit of opportunities to leverage innovative technology to bring more efficiency, value and customer satisfaction to U.S. Healthcare
Gain Regulatory Compliance